What is Hepatitis A?
By: Archiradhi Communications
- Introduction
- Characteristics, Immunity, and Rare Complications
- Main Modes of Transmission
- Key Risk Factors
- Immune Response and Liver Injury
- Clinical Presentation
- Common Laboratory Results
- Contagious Period and Viral Shedding
- Recovery and Long-Term Outlook
- Fulminant Hepatic Failure: Characteristics and Implications
- The Extrahepatic Manifestations of HAV Infection
- Clinical Observations of Relapse
- Prolonged Cholestasis
- Clinical and Laboratory Diagnosis
- Treatment and Vaccination
- Conclusion
Introduction
Hepatitis is a broad term encompassing liver inflammation. The causes of hepatitis may be either infectious or noninfectious.
Infectious causes include a diverse range of bacterial, viral, fungal, and parasitic pathogens. Noninfectious factors contributing to hepatitis include metabolic diseases, autoimmune disorders, certain drugs, and alcohol.
There are five main types of hepatitis viruses- A, B, C, D, and E. Despite the fact that they all cause liver disease, they significantly differ in terms of transmission, disease severity, geographical prevalence, and preventive strategies.
Types B and C are particularly concerning because they have the potential to cause chronic liver disease in a significant number of individuals, making them the leading causes of liver cirrhosis, and hepatitis-related deaths.
Hepatitis B Virus
Approximately 354 million people are currently living with hepatitis B or C worldwide.
Other lesser-known causes of viral hepatitis are cytomegalovirus, Epstein-Barr virus, herpes simplex virus, and adenovirus.
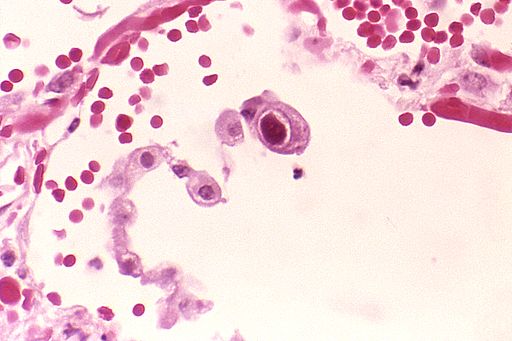
Cytomegalovirus
In this article, we will delve into the world of Hepatitis A Virus Infection.
Characteristics, Immunity, and Rare Complications
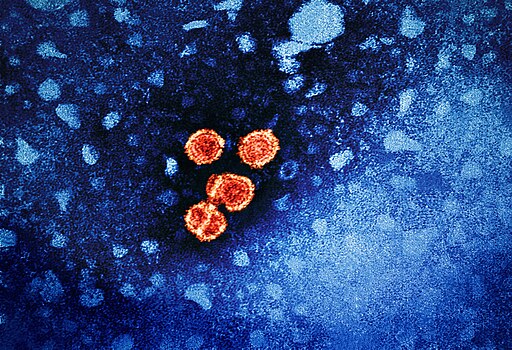
Hepatitis A Virus (HAV) is responsible for causing hepatitis A infection. It comes under the Hepatovirus genus within the Picornaviridae family.
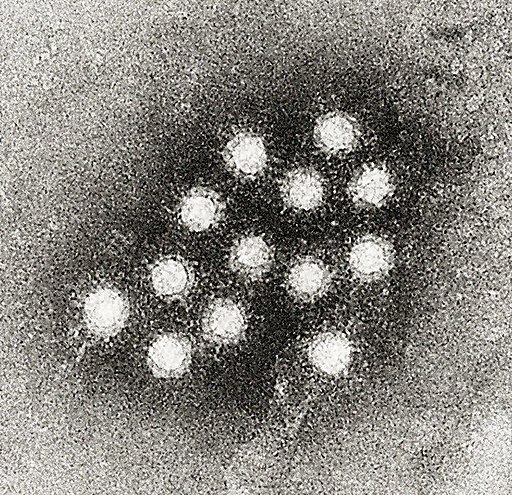
Hepatitis A Virus
Humans serve as the sole reservoir for this virus. Infection is typically self-limiting and grants lifelong immunity. Fortunately, vaccination effectively prevents the disease.
In very rare instances, fulminant hepatic failure may occur.
Main Modes of Transmission
The chief mode of transmission is through the fecal-oral route.
This typically results from the consumption of contaminated food or water such as raw or
undercooked vegetables, shellfish, or food handled by infected food handlers.
Moreover, person-to-person contact, particularly within households, daycare centers, and other close settings can contribute to infection spread.
To date, there have been no observed cases of maternal-to-fetal transmission.
Key Risk Factors
Individuals aged above 50 years are at higher risk of contracting hepatitis A infection. Those with underlying liver disease, especially chronic hepatitis C virus infection, are also at increased risk.
Immune Response and Liver Injury
The liver sustains injury as a result of the body’s immune response to viral replication within the hepatocyte cytoplasm.
This immune reaction involves specialized cells known as human leukocyte antigen-restricted, HAV-specific CD8+ lymphocytes and natural killer cells.
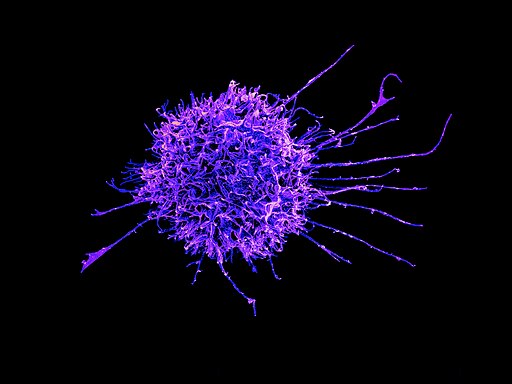
Natural Killer Cells
Interferon-gamma also plays a crucial role in clearing the infected hepatocytes.
In certain cases, an excessive host response can occur, resulting in severe hepatitis. This causes pronounced liver damage.
Clinical Presentation
Symptoms are uncommon in children under the age of six. In adults, acute HAV infection is typically a self-limited illness.
Less than one percent of cases will progress to fulminant hepatic failure.
The incubation period lasts around 28 days (range 15-50 days).
In over 70 percent of affected adults, symptomatic illness occurs. This is characterized by a sudden onset of fever, nausea, anorexia, vomiting, abdominal pain, and malaise.
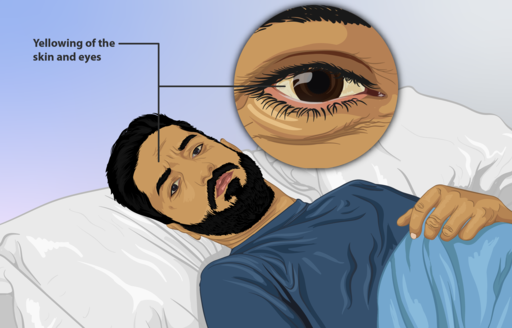
Dark colored urine (called bilirubinuria) and pale stools (absence of bilirubin pigment) are seen within a few days to a week.
Subsequently, jaundice and pruritus may occur in up to 70 percent of infections. With the appearance of jaundice, the early signs and symptoms reduce.
Acute infection in pregnant women has been linked to a greater risk of preterm labor and gestational complications.
Common Laboratory Results
Laboratory tests reveal elevated serum aminotransferases (usually above 1000 international units/dL), serum bilirubin levels less than or equal to 10 mg/dL, and alkaline phosphatase levels up to 400 U/L.
Contagious Period and Viral Shedding
Infected individuals can spread the virus during the incubation period and for approximately one week after jaundice becomes evident.
The virus actively multiplies in the liver and is released in high concentrations in stool, two to three weeks before the appearance of clinical symptoms
Recovery and Long-Term Outlook
In over 80 percent of patients, full recovery is observed within two to three months. Almost all patients will achieve complete recovery within six months.
It is important to note that HAV infection does not become chronic. While patients are safe from reinfection, relapses can arise.
Fulminant Hepatic Failure: Characteristics and Implications
Fulminant hepatic failure is characterized by the onset of severe acute liver injury.
This culminates in encephalopathy and impaired synthetic function. Individuals with existing liver diseases (such as hepatitis B or C) and those aged over 50 years are predominantly affected.
In certain cases, a liver transplant may become necessary for optimal treatment and recovery.
The Extrahepatic Manifestations of HAV Infection
Apart from hepatic involvement, HAV is also associated with several extrahepatic manifestations such as arthralgias and evanescent rash.
Such occurrences are more common in patients who experience protracted illnesses such as relapsing or cholestatic hepatitis.
Clinical Observations of Relapse
Within six months of acute illness, around ten percent of patients will experience a relapse of symptoms.
This clinical relapse usually lasts less than three weeks, whereas the biochemical markers of relapse may persist for a year.
It should be noted here that an individual can suffer from multiple relapses during their lifetime. However, complete recovery is the norm.
Prolonged Cholestasis
When jaundice persists for more than three months, it is categorized as prolonged cholestasis. Less than five percent of patients are affected.
This condition is characterized by pronounced jaundice, weight loss, diarrhea, pruritus, and fever. However, the resolution is spontaneous in most cases.
There are no lasting sequelae.
Clinical and Laboratory Diagnosis
Anorexia, nausea, fever, abdominal pain, elevated serum aminotransferase levels, and jaundice should raise suspicion of HAV infection.
Serum IgM anti-HAV antibodies are used to establish diagnosis. They can be identified from the onset of symptoms and reach their peak during the acute phase of the infection. These antibodies persist in instances of relapsing hepatitis.
The presence of serum IgG anti-HAV antibodies implies lifelong protective immunity.
Treatment and Vaccination
Fulminant hepatic failure necessitates intensive supportive therapy. Otherwise, HAV infection is self-limited and supportive care is sufficient.
Relevant guidelines for vaccination against HAV are provided by reputable sources such as the World Health Organization and the United States Centers for Disease Control and Prevention.
Currently available Hepatitis A vaccines include VAQTA, HAVRIX, TWINRIX, VIATIM, VIVAXIM, BIOVAC-A, and MEDVAC-A. These vaccines are both efficacious and well-tolerated.
This diverse range includes single-antigen inactivated hepatitis A vaccines (VAQTA, HAVRIX), combination vaccines for hepatitis A and B (TWINRIX), and formulations providing protection against both hepatitis A and typhoid (VIATIM, VIVAXIM).
Additionally, live attenuated hepatitis A vaccines such as BIOVAC-A and MEDVAC-A are available in different regions across the globe.
Conclusion
As we conclude our exploration of the world of Hepatitis A, let us remind ourselves once again the importance of safeguarding our liver health.
The impact of viral hepatitis can be devastating, silently wreaking havoc on our bodies until it reaches an advanced stage.
By educating ourselves and our loved ones about viral hepatitis, encouraging vaccination, and promoting healthy practices, we can work towards a world where every life is cherished, and every liver is protected.